Know how to calculate case mix index. The Case Mix Index (CMI) is a critical metric in healthcare that reflects the average severity and complexity of patients treated at a hospital. It plays a pivotal role in determining reimbursement rates, evaluating hospital performance, and allocating resources effectively. But how exactly is this metric calculated? In this comprehensive guide, we’ll break down the formula, explain its components, and explore why it matters for healthcare providers.
What Is the Case Mix Index (CMI)?
The Case Mix Index is a numerical value that quantifies the average relative diagnosis-related group (DRG) weight for all patients discharged from a hospital during a specific period. Each DRG is assigned a weight by the Centers for Medicare & Medicaid Services (CMS), representing the resource intensity required to treat patients within that category. A higher CMI indicates a hospital treats more complex cases, while a lower CMI suggests less resource-intensive care.
Why Is CMI Important?
1. Reimbursement Determination
Medicare, Medicaid, and private insurers use CMI to adjust payment rates. Hospitals with higher CMIs typically receive higher reimbursements.
2.Benchmarking Performance
CMI helps compare hospitals’ patient populations and efficiency.
3.Resource Allocation
It aids in staffing decisions, budgeting, and infrastructure planning.
4. Quality Reporting
Regulatory bodies use CMI to assess risk-adjusted outcomes.
The Role of DRGs in Calculating CMI
Diagnosis-Related Groups (DRGs) are the foundation of CMI. Each DRG categorizes patients based on diagnoses, procedures, age, and discharge status. For example:
- A simple pneumonia case might fall under DRG 193 (weight = 1.2).
- A complex heart surgery could be DRG 231 (weight = 5.8).
CMS updates DRG weights annually, reflecting changes in treatment costs and medical advancements.
Step-by-Step Formula for how to calculate case mix index
To calculate CMI, follow these steps:
Step 1: Identify All Discharges and Their DRG Weights
Compile data for all patient discharges during a specific period (e.g., a month or year). For each discharge, note the corresponding DRG code and its assigned weight.
Step 2: Sum All DRG Weights
Add the DRG weights of every patient case. For example:
- 10 cases of DRG 193 (1.2 each) = 12.0
- 5 cases of DRG 231 (5.8 each) = 29.0
- Total DRG Weight = 12.0 + 29.0 = 41.0
Step 3: Count Total Number of Discharges
Tally the total number of patients discharged. In the example above:
10 + 5 = 15 discharges
Step 4: Divide Total DRG Weight by Total Discharges
Use the formula:
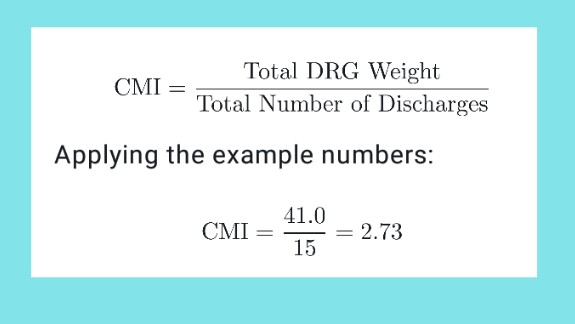
This means the average patient case at this hospital has a DRG weight of 2.73, indicating moderately high complexity.
Real-World Example of CMI Calculation
Let’s consider a hospital with 1,000 discharges in a year:
| DRG Code | Number of Cases | DRG Weight | Total Weight per DRG |
| 123 | 200 | 0.8 | 160 |
| 456 | 300 | 1.5 | 450 |
| 789 | 500 | 2.3 | 1150 |
Total DRG Weight= 160 + 450 + 1,150 = 1,760
Total Discharges = 200 + 300 + 500 = 1,000
CMI = 1,760 / 1,000 = 1.76
This hospital’s CMI of 1.76 suggests it handles cases requiring 76% more resources than the “average” hospital (which has a baseline CMI of 1.0).
Factors That Influence Case Mix Index
1.Patient Acuity: Hospitals specializing in trauma, oncology, or transplants typically have higher CMIs.
2.Coding Accuracy: Incorrect DRG assignments due to documentation errors can skew CMI.
3.Service Offerings: Facilities offering advanced surgeries or neonatal care often report higher CMIs.
4.Discharge Volume: A sudden surge in low-severity cases (e.g., flu outbreaks) may temporarily lower CMI.
Why Accurate CMI Calculation Matters
Financial Impact: Underreporting complexity can lead to lost revenue, while overreporting risks audits and penalties.
Strategic Planning: A rising CMI may signal the need for more specialists or equipment.
Quality Metrics: CMS uses CMI to adjust readmission rates and mortality data, ensuring fair comparisons between hospitals.
Challenges in Calculating CMI
1. DRG Misclassification: Errors in coding diagnoses or procedures distort weights.
2. Data Timeliness: Delays in updating DRG databases affect accuracy.
3. Changing Regulations: Annual updates to DRG weights require hospitals to adapt quickly.
Best Practices for Optimizing CMI
- Invest in Staff Training: Ensure coding teams understand ICD-10 and DRG guidelines.
- Audit Regularly: Conduct internal reviews to catch coding errors.
- Leverage Technology: Use EHR systems with built-in DRG validation tools.
- Monitor Trends: Track CMI quarterly to identify shifts in patient demographics.
Calculating the Case Mix Index is essential for hospitals to secure fair reimbursements, maintain operational efficiency, and deliver high-quality care. By accurately summing DRG weights and dividing by total discharges, healthcare providers gain insights into their patient population’s complexity. However, success hinges on precise coding, continuous monitoring, and adapting to regulatory changes.
Understanding your hospital’s CMI isn’t just about numbers—it’s about leveraging data to improve patient outcomes and financial sustainability. Whether you’re a hospital administrator, coder, or clinician, mastering this metric empowers you to make informed decisions in an evolving healthcare landscape.
read more
